Patient Resources
RMA of New York – Long Island is proud to offer a comprehensive library of patient resources that are tailored to support and inform you throughout your fertility journey. Whether you're looking to expand your knowledge of fertility terms or want to conduct your own research, our patient resources can provide additional support throughout your fertility journey.

Blog & Podcasts
Stay up-to-date with the latest fertility news, research, and updates from our team of physicians and fertility specialists at RMA of New York.

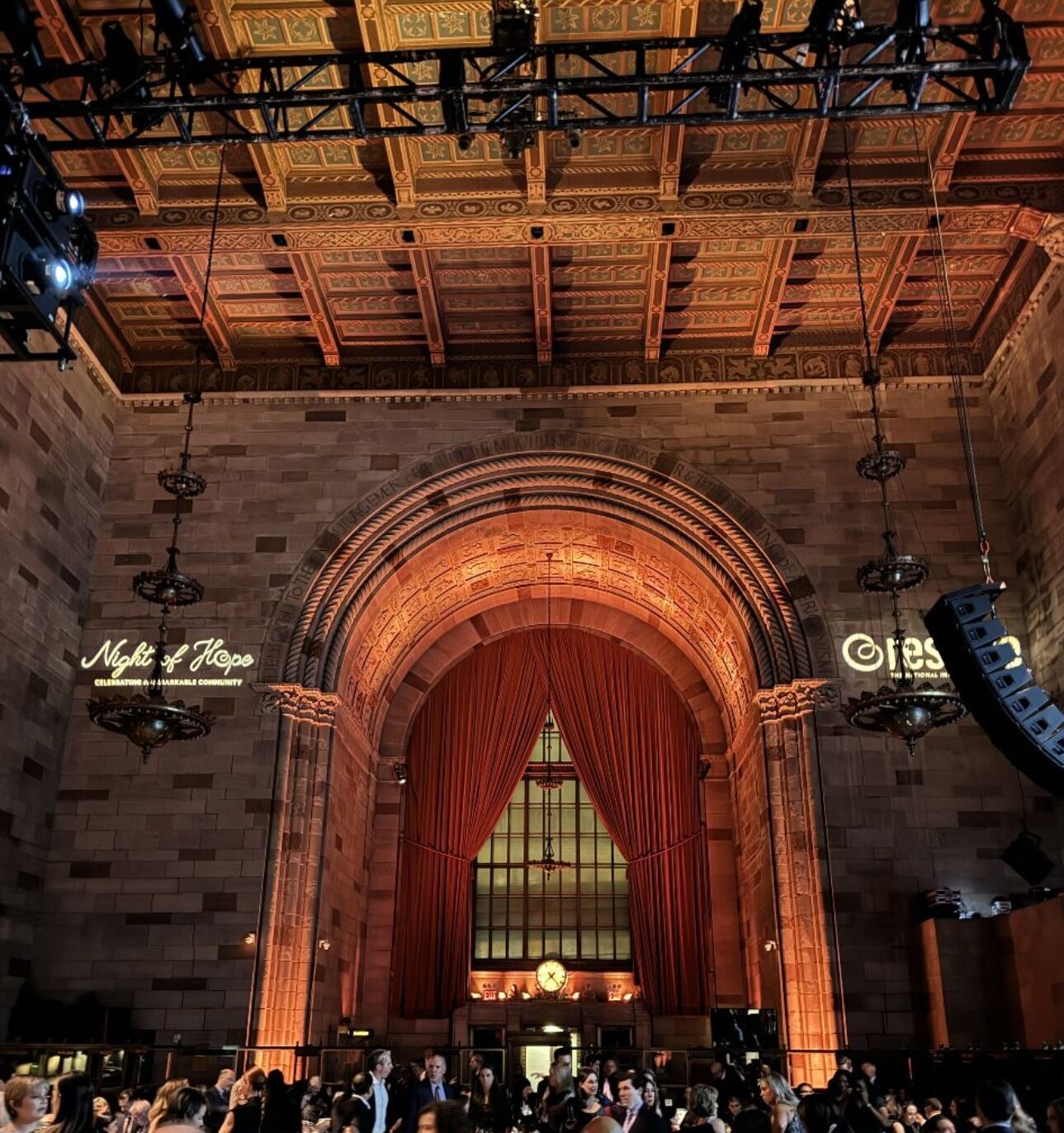
Events Calendar
You're invited to join us at RMA of New York – Long Island for live and virtual fertility educational events, and other community activities.
Get Started
It’s never too early to learn about your fertility and reproductive options.
Have questions? We can help.
Patient-centric reproductive medicine is our specialty, and we look forward to answering any questions you may have.